Obsessive-Compulsive Personality Disorder (OCPD)
Understanding the symptoms and getting help for you or a loved one

Are obsessive thoughts and compulsive behaviors interfering with your daily life? Explore the symptoms, treatment, and self-help for OCD.

It’s normal, on occasion, to go back and double-check that the iron is unplugged or worry that you might be contaminated by germs, or even have an occasional unpleasant, violent thought. But if you suffer from obsessive-compulsive disorder (OCD), obsessive thoughts and compulsive behaviors become so consuming they interfere with your daily life.
OCD is characterized by uncontrollable, unwanted thoughts and ritualized, repetitive behaviors you feel compelled to perform. If you have OCD, you probably recognize that your obsessive thoughts and compulsive behaviors are irrational—but even so, you feel unable to resist them and break free.
Like a needle getting stuck on an old record, OCD causes the brain to get stuck on a particular thought or urge. For example, you may check the stove 20 times to make sure it’s really turned off because you’re terrified of burning down your house, or wash your hands until they’re scrubbed raw for fear of germs. While you don’t derive any sense of pleasure from performing these repetitive behaviors, they may offer some passing relief for the anxiety generated by the obsessive thoughts.
You may try to avoid situations that trigger or worsen your symptoms or self-medicate with alcohol or drugs. But while it can seem like there’s no escaping your obsessions and compulsions, there are plenty of things you can do to break free of unwanted thoughts and irrational urges and regain control of your thoughts and actions.
Historically, OCD was categorized as an anxiety disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM). However, in the fifth edition, the DSM separated OCD from the “Anxiety Disorders” section and created a new section called “Obsessive-Compulsive and Related Conditions.”
The change was made after researchers noted important differences between OCD and anxiety disorders. For example, with OCD you respond to unwanted thoughts with repetitive, unhelpful rituals. You may or may not realize that your thoughts and compulsions, such as excessive hand washing, are irrational. With anxiety, though, you're more likely to ruminate over real-world concerns, such as a fear of being mocked or judged. You may respond by avoiding the source of your fear, but won’t use odd rituals to ease your distress.
Certain interventions for OCD and anxiety disorders can also differ. To deal with an anxiety disorder, you might need to practice gradually facing your fears, whereas with OCD, it’s also important to address the compulsive behavior.
BetterHelp is an online therapy service that matches you to licensed, accredited therapists who can help with depression, anxiety, relationships, and more. Take the assessment and get matched with a therapist in as little as 48 hours.
Take Assessment HelpGuide is user supported. We may earn a commission if you sign up for BetterHelp’s services after clicking through from this site. Learn moreObsessions are involuntary thoughts, images, or impulses that occur over and over again in your mind. You don't want to have these ideas, but you can't stop them. Unfortunately, these obsessive thoughts are often disturbing and distracting.
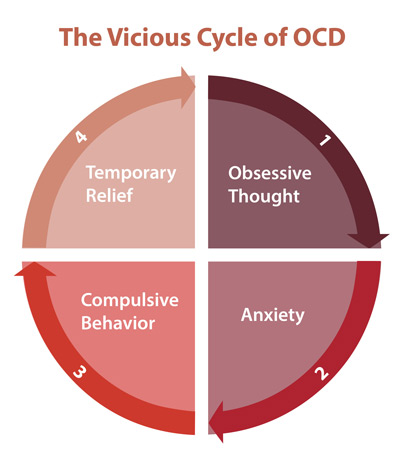
Compulsions are behaviors or rituals that you feel driven to act out again and again. Usually, compulsions are performed in an attempt to make obsessions go away. For example, if you're afraid of contamination, you might develop elaborate cleaning rituals. However, the relief never lasts. In fact, the obsessive thoughts usually come back stronger. And the compulsive rituals and behaviors often end up causing anxiety themselves as they become more demanding and time-consuming. This is the vicious cycle of OCD.
Hoarding used to be considered a category of OCD. While estimates suggest that up to 25 percent of people with OCD experience compulsive hoarding, it can also be a sign of a separate condition, hoarding disorder.
Hoarders fear that something bad will happen if they throw anything away and hoard things that they don’t need or use. However, there are distinctions between OCD-related hoarding and hoarding disorder.
OCD-related hoarders tend not to accumulate so many possessions that their homes become unmanageable. Hoarding for them is usually unwelcome and distressing—a way to manage intrusive thoughts.
Someone with hoarding disorder, on the other hand, experiences both positive and negative emotions. Acquiring possessions provides pleasure rather than simply satisfying a compulsion and they being surrounded by their things provides comfort. The distress in hoarding disorder stems more from the consequences of hoarding—the clutter and unsafe environment—along with the anxiety of having to discard possessions.
Read: Hoarding Disorder: Help for Hoarders.
Just because you have obsessive thoughts or perform compulsive behaviors does NOT mean that you have obsessive-compulsive disorder. With OCD, these thoughts and behaviors cause tremendous distress, take up a lot of time (at least one hour per day), and interfere with your daily life and relationships.
Most people with obsessive-compulsive disorder have both obsessions and compulsions, but some people experience just one or the other.
While the onset of obsessive-compulsive disorder usually occurs during adolescence or young adulthood, younger children sometimes have symptoms that look like OCD. However, the symptoms of other disorders, such as ADHD, autism, and Tourette's syndrome, can also look like obsessive-compulsive disorder, so a thorough medical and psychological exam is essential before any diagnosis is made.
The sudden development of intense OCD symptoms can also be a sign of pediatric acute-onset neuropsychiatric syndrome (PANS) or pediatric autoimmune neuropsychiatric disorder associated with streptococcal infections (PANDAS).
Read: PANS and PANDAS: Acute-Onset OCD in Children.
The first step to managing your OCD symptoms is to recognize the triggers—the thoughts or situations—that bring on your obsessions and compulsions. Record a list of the triggers you experience each day and the obsessions they provoke. Rate the intensity of the fear or anxiety you experienced in each situation and then the compulsions or mental strategies you used to ease your anxiety. For example, if you have a fear of being contaminated by germs, touching a railing at the mall might generate a fear intensity of 3, whereas touching the restroom floor in the mall might generate a 10 and require 15 minutes of hand washing to ease your anxiety.
Keeping track of your triggers can help you anticipate your urges. And by anticipating your compulsive urges before they arise, you can help to ease them. For example, if your compulsive behavior involves checking that doors are locked, windows closed, or appliances turned off, try to lock the door or turn off the appliance with extra attention the first time.
Identifying and recording your triggers also provides an important tool for learning to resist your OCD compulsions.
It might seem smart to avoid the situations that trigger your obsessive thoughts, but the more you avoid them, the scarier they feel. Conversely, by repeatedly exposing yourself to your OCD triggers, you can learn to resist the urge to complete your compulsive rituals. This is known as exposure and response prevention (ERP) and is a mainstay of professional therapy for OCD.
ERP requires you to repeatedly expose yourself to the source of your obsession—and then refrain from the compulsive behavior you’d usually perform to reduce your anxiety. If you are a compulsive hand washer, for example, that could mean touching the door handle in a public restroom and then not allowing yourself to wash your hands. As you sit with the anxiety, the urge to wash your hands will gradually begin to go away on its own. In this way, you’ll learn that you don’t need the ritual to get rid of your anxiety and that you have some control over your obsessive thoughts and compulsive behaviors.
Tackling your biggest fears straight off might be too extreme, so ERP exercises start with you confronting lesser fears and then working your way up the “fear ladder.” Confront those situations that generate a low fear intensity and once you’re able to tolerate the anxiety you can move on to the next, more difficult exposure challenge.
Think about your end goal (to be able to use a public restroom without fear of contamination, for example, or to drive to work without stopping to check if you’ve hit something) and then break down the steps needed to reach that goal. Using the information you recorded in identifying your triggers, make a list of situations from the least scary to the most scary. The first step should make you slightly anxious, but not so frightened that you’re too intimidated to try it.
Here's a sample fear ladder:
| Fear intensity | Situation |
|---|---|
| 10 | Drive all the way to work without stopping to check if you've hit something |
| 8 | Don’t phone your spouse to check they got to work safely |
| 6 | Leave the house, lock the front door and walk away without checking |
| 4 | Turn off the stove and leave the room without checking |
| 2 | Put milk in the refrigerator without checking the top is secure |
Work your way up the ladder. Start with the first step and don’t move on until you start to feel more comfortable doing it. If possible, stay in the situation long enough for your anxiety to decrease. The longer you expose yourself to your OCD trigger, the more you’ll get used to it and the less anxious you’ll feel when you face it the next time. Once you’ve done a step on several separate occasions without feeling too much anxiety, you can move on to the next step. If a step is too hard, break it down into smaller steps or go slower.
As you’re resisting your compulsions, focus on the feelings of anxiety. Instead of trying to distract yourself, allow yourself to feel anxious as you resist the urge to engage in your compulsive behavior. You may believe that the discomfort you’re feeling will continue until you engage in the compulsion. But if you stick with it, the anxiety will fade. And you’ll realize that you’re not going to “lose control” or have some kind of breakdown if you don’t perform the ritual.
Practice. The more often you practice, the quicker your progress will be. But don’t rush. Go at a pace that you can manage without feeling overwhelmed. And remember: you will feel uncomfortable and anxious as you face your fears, but the feelings are only temporary. Each time you expose yourself to your trigger, your anxiety should lessen and you’ll start to realize that you have more control (and less to fear) than you thought.
Everyone has troubling thoughts or worries from time to time. But obsessive-compulsive disorder causes the brain to get stuck on a particular anxiety-provoking thought, causing it to play over and over in your head. The more unpleasant or distressing the thought, the more likely you are to try to repress it. But repressing thoughts is almost impossible and trying usually has the opposite effect, causing the unpleasant thought to resurface more frequently and become more bothersome.
As with resisting compulsions, you can overcome disturbing, obsessive thoughts by learning to tolerate them through exposure and response prevention exercises. It’s also important to remind yourself that just because you have an unpleasant thought, that doesn’t make you a bad person. Your thoughts are just thoughts. Even unwanted, intrusive, or violent thoughts are normal—it’s only the importance you attach to them that turns them into damaging obsessions.
The following strategies can help you see your thoughts for what they are and regain a sense of control over your anxious mind.
Keep a pad and pencil on you, or type on a smartphone. When you begin to obsess, write down all your thoughts or compulsions.
Rather than trying to suppress obsessions or compulsions, develop the habit of rescheduling them.
Use your worry period to challenge negative or intrusive thoughts by asking yourself:
Focus on one specific thought or obsession and record it to a tape recorder or smartphone.
OCD can get worse when you feel powerless and alone, so it’s important to build a strong support system. The more connected you are to other people, the less vulnerable you’ll feel. And just talking to an understanding person about your worries and urges can make them seem less threatening.
Stay connected to family and friends. Obsessions and compulsions can consume your life to the point of social isolation. In turn, social isolation will aggravate your OCD symptoms. It’s important to invest in relating to family and friends. Talking face-to-face about your worries and urges can make them feel less real and less threatening.
Join an OCD support group. You’re not alone in your struggle with OCD, and participating in a support group can be an effective reminder of that. OCD support groups enable you to both share your own experiences and learn from others who are facing the same problems.
While stress doesn’t cause OCD, it can trigger symptoms or make them worse. Physical exercise and connecting with another person face-to-face are two very effective ways to calm your nervous system. You can also:
Quickly self-soothe and relieve anxiety symptoms by making use of one or more of your physical senses—sight, smell, hearing, touch, taste—or movement. You might try listening to a favorite piece of music, looking at a treasured photo, savoring a cup of tea, or stroking a pet.
Practice relaxation techniques. Mindful meditation, yoga, deep breathing, and other relaxation techniques can help lower your overall stress and tension levels and help you manage your urges. For best results, try practicing a relaxation technique regularly.
A healthy, balanced lifestyle plays a big role in easing anxiety and keeping OCD compulsions, fears, and worry at bay.
Exercise regularly. Exercise is a natural and effective anti-anxiety treatment that helps to control OCD symptoms by refocusing your mind when obsessive thoughts and compulsions arise. For maximum benefit, try to get 30 minutes or more of aerobic activity on most days. Ten minutes several times a day can be as effective as one longer period especially if you pay mindful attention to the movement process.
Get enough sleep. Not only can anxiety and worry cause insomnia, but a lack of sleep can also exacerbate anxious thoughts and feelings. When you're well rested, it's much easier to keep your emotional balance, a key factor in coping with anxiety disorders such as OCD.
Avoid alcohol and nicotine. Alcohol temporarily reduces anxiety and worry, but it actually causes anxiety symptoms as it wears off. Similarly, while it may seem that cigarettes are calming, nicotine is actually a powerful stimulant. Smoking leads to higher, not lower, levels of anxiety and OCD symptoms.
Cognitive-behavioral therapy is the most effective treatment for obsessive-compulsive disorder and generally involves two components:
In addition to cognitive-behavioral therapy, the following treatments are also used for OCD:
Medication. Antidepressants are sometimes used in conjunction with therapy for the treatment of obsessive-compulsive disorder. However, medication alone is rarely effective in relieving the symptoms.
Family Therapy. Since OCD often causes problems in family life and social adjustment, family therapy can help promote understanding of the disorder and reduce family conflicts. It can also motivate family members and teach them how to help their loved one with OCD.
Group Therapy. Through interaction with fellow OCD sufferers, group therapy provides support and encouragement and decreases feelings of isolation.
In some people, OCD symptoms such as compulsive washing or hoarding are ways of coping with trauma. If you have post-traumatic OCD, cognitive approaches may not be effective until underlying traumatic issues are resolved.
The way you react to your loved one's OCD symptoms can have a big impact on their outlook and recovery. Negative comments or criticism can make OCD worse, while a calm, supportive environment can help improve the outcome of treatment.
Avoid making personal criticisms. Remember, your loved one's OCD behaviors are symptoms, not character flaws.
Don't scold someone with OCD or tell them to stop performing rituals. They can't comply, and the pressure to stop will only make the behaviors worse.
Be as kind and patient as possible. Each sufferer needs to overcome problems at their own pace. Praise any successful attempt to resist OCD, and focus attention on positive elements in the person's life.
Do not play along with your loved one’s rituals. Going along with your loved one’s OCD “rules,” or helping with their compulsions or rituals will only reinforce the behavior. Support the person, not their compulsions.
Keep communication positive and clear. Communication is important so you can find a balance between supporting your loved one and standing up to the OCD symptoms and not further distressing your loved one.
Find the humor. Laughing together over the funny side and absurdity of some OCD symptoms can help your loved one become more detached from the disorder. Just make sure your loved one feels respected and in on the joke.
Don't let OCD take over family life. Sit down as a family and decide how you will work together to tackle your loved one's symptoms. Try to keep family life as normal as possible and the home a low-stress environment.
Call the NAMI Helpline at 1-800-950-6264. Or Find a Therapist.
Call Anxiety UK at 03444 775 774.
Find services at Anxiety Canada.
Call the SANE Help Centre at 1800 18 7263.
Call the Vandrevala Foundation at 1860 2662 345 or 1800 2333 330.
Access a global database of OCD resources from the International OCD Foundation.
Millions of readers rely on HelpGuide.org for free, evidence-based resources to understand and navigate mental health challenges. Please donate today to help us save, support, and change lives.
Donate to HelpGuide.org today